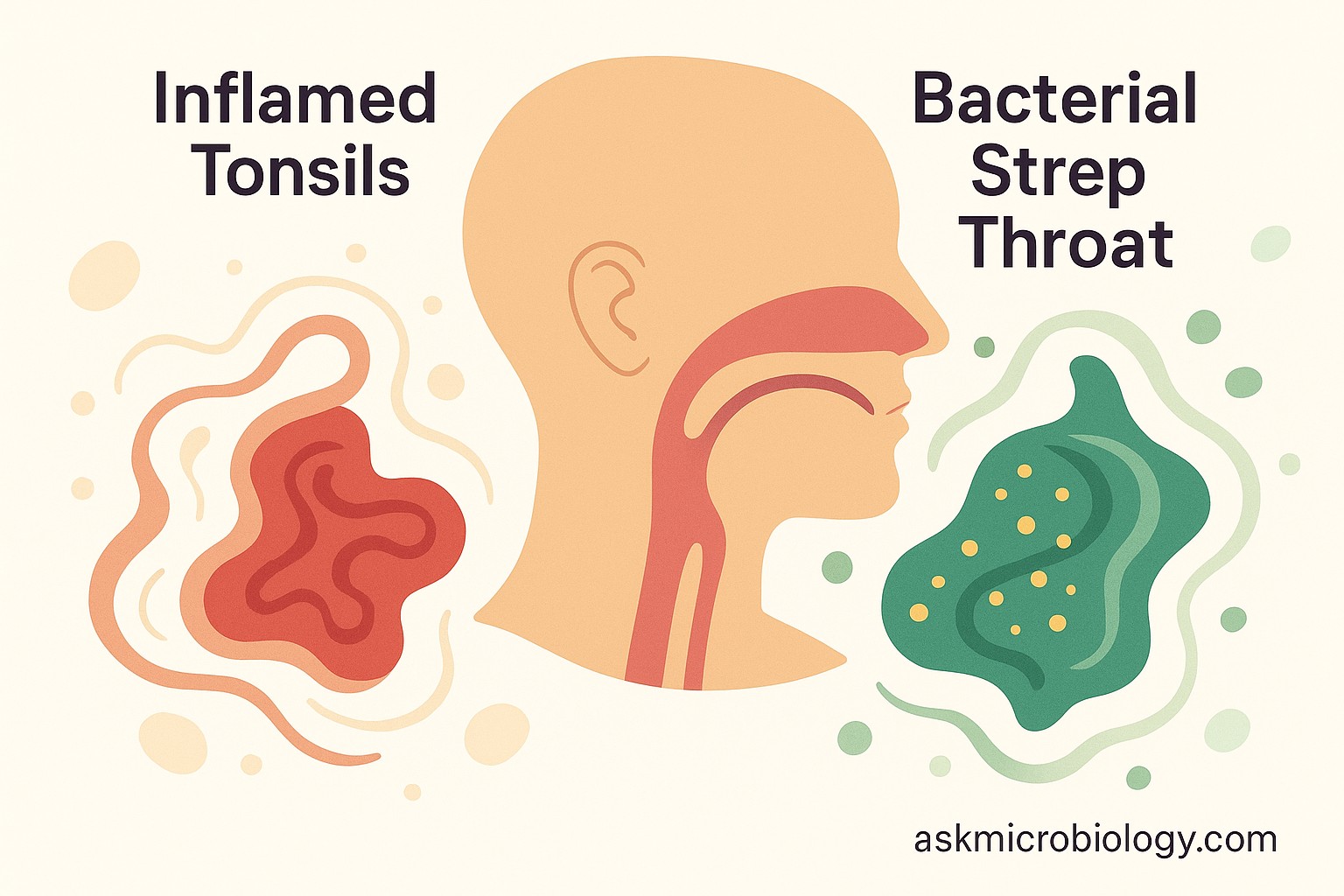
Sore throats can be confusing. You might hear a doctor say “it looks like tonsillitis,” while someone else mentions “strep throat,” and you’re left wondering – what’s the difference? The truth is, strep throat and tonsillitis are closely related, but not the same thing. Think of tonsillitis as a general condition (inflamed, infected tonsils) and strep throat as one specific cause of that condition (a particular bacteria causing a throat infection). Many of the symptoms overlap, which is why people mix up the terms. In this quick guide, we’ll compare strep throat and tonsillitis in simple terms, covering what causes each, how the symptoms may differ, and what to expect for treatment. By the end, you’ll understand how these two are connected and why the distinction matters for getting the right care.
Different Causes: One Bacteria vs. Many Possible Germs
The biggest difference between tonsillitis and strep throat lies in what’s causing the infection:
- Tonsillitis means inflammation of the tonsils, usually due to an infection. But that infection could be caused by a variety of germs, most often viruses. In fact, most tonsillitis in children and adults is triggered by common viruses – the kinds that also cause colds and flus. It can also be caused by bacteria (and when it is, the most likely bacterial culprit is… you guessed it: strep). So, tonsillitis is a broad term. If your tonsils are red, swollen, and painful, you have tonsillitis – but we still need to figure out which germ is behind it.
- Strep throat is short for streptococcal pharyngitis. It is an infection of the throat (including the tonsils) specifically caused by Group A Streptococcus bacteria. This is a very particular germ. Essentially, strep throat is a type of tonsillitis – the kind that’s caused by bacteria rather than a virus. To put it another way, if you have strep throat, you have tonsillitis (because your tonsils are infected and inflamed). But you can have tonsillitis without it being strep throat (for example, if a virus is to blame). Many people find this confusing at first. A helpful analogy: Think of tonsillitis as an “umbrella” term for inflamed tonsils. Strep throat falls under that umbrella as one specific scenario.
One way to look at it: all strep throat cases are tonsillitis, but not all tonsillitis is strep throat. There are other bacteria and many viruses that can infect the tonsils. That said, strep bacteria are among the most common and important causes, especially in kids. Group A Strep is responsible for roughly 20-30% of tonsillitis cases in children, with the rest being mostly viral. Knowing the cause is important because it directs the treatment (antibiotics help bacterial infections like strep, but won’t do anything for a virus).
Symptom Comparison: How to Tell Which One You Have
Because strep throat is one type of tonsillitis, it’s no surprise that they share many symptoms. Both can cause a very sore throat, redness of the tonsils, pain when swallowing, swollen neck lymph nodes, and fever. However, there are a few clues that doctors (and you) can look for to differentiate a likely strep throat from a viral tonsillitis:
- Presence or absence of cold symptoms: If you have a cough, runny or stuffy nose, or sneezing, those suggest a viral infection (and thus viral tonsillitis). Strep throat usually does not cause cough or runny nose. So, a sore throat accompanied by sniffles and cough is more likely due to a virus – maybe a bad cold affecting your throat. On the flip side, if your throat is extremely sore but your nose is clear and you’re not coughing, strep is more suspicious.
- Severity of throat pain and swallowing trouble: Strep throat often comes on fast and can be quite painful, sometimes making swallowing very difficult. Tonsillitis from a virus can also hurt, but strep tends to be one of the worst in terms of throat pain. Children with strep may complain that it hurts too much to swallow even saliva, or they might start drooling because they’re avoiding swallowing. If a child is drooling and refusing to eat due to throat pain, that’s a red flag and a doctor will definitely check for strep.
- Fever level: Both viral and strep can cause fever, but high fever (above 101°F or 38.3°C) is a bit more common with strep throat. Viral tonsillitis (like in a common cold) might cause a mild or moderate fever or none at all. If you have a high fever along with throat pain and no cough, we think more about strep.
- Tonsil appearance: In both types, your tonsils will likely be red and swollen. White or yellow patches (pus) on the tonsils can occur in strep throat and sometimes in severe viral infections too (so it’s not a slam-dunk distinction, but pus points toward bacterial). Strep can cause the tonsils to have white streaks or spots of pus; doctors look for this during the exam. Viral tonsillitis often doesn’t have pus, though something like mononucleosis (a viral illness) can produce a grayish-white coating on the tonsils. So, presence of pus = possibly strep, absence of pus doesn’t rule strep out but is a clue.
- Other body symptoms: Strep throat can sometimes come with some unique extras. Some people with strep develop a sandpapery red rash on their body called scarlet fever (caused by toxins from the bacteria). Strep can also cause headache, belly pain, nausea, or even vomiting, especially in kids. Viral infections might cause more classic cold symptoms like body aches or ear pain or hoarseness. If you have hoarse voice or lots of congestion, that leans viral. If you have rash or stomach pain with your sore throat, that leans strep/bacterial.
Even with these clues, it’s often not possible to be 100% certain just from symptoms. Doctors often do a rapid strep test because guessing isn’t good enough if strep is a possibility. The test can confirm strep in minutes. If it’s negative but suspicion is high, a throat culture (which takes a day or two) might be done to double-check.
Diagnosis: How Doctors Confirm What It Is
- Strep Throat Diagnosis: If strep is suspected, a nurse or doctor will swab your throat (quickly brushing the tonsils/back of throat with a long Q-tip). This can cause a brief gag, but it’s over fast. The swab is tested for the presence of Group A Streptococcus bacteria. A rapid antigen test can give results in about 5-10 minutes. If it’s positive, you have strep throat – no further questions. If it’s negative and they still think it might be strep (maybe because your symptoms are textbook or there’s a known outbreak at home or school), they will send a throat culture to the lab. The culture is very sensitive and will catch cases the rapid test might miss. It takes 1-2 days for results. This is the gold standard for diagnosis. There’s no equivalent “rapid test” for every virus; often if strep is ruled out, doctors assume a virus is causing the tonsillitis.
- Tonsillitis (General) Diagnosis: For tonsillitis that isn’t obviously strep, diagnosis is more about ruling things out and ensuring no serious complications. The doctor examines the throat, asks about symptoms, and might test for strep or sometimes test for mononucleosis if symptoms fit (mono can cause severe tonsillitis in teens). If all tests are negative, usually the conclusion is it’s a viral infection causing the tonsillitis. Specific viruses usually don’t need to be identified (they often can’t be easily, and it wouldn’t change treatment).
In short, diagnosing strep throat involves a specific test for the strep bacteria, whereas diagnosing viral tonsillitis means making sure strep isn’t present and then treating it as a viral illness.
Treatment Differences: Antibiotics or Not?
This is where knowing the difference really matters:
- Treatment for Strep Throat: Because strep throat is a bacterial infection, it is treated with antibiotics. Penicillin or amoxicillin are common choices, but other antibiotics can be used if you’re allergic or if the situation calls for it. Antibiotics do a few important things: they shorten the illness (you’ll start feeling better in a day or two), they prevent complications (like rheumatic fever, which can happen if strep is left untreated), and they make you not contagious faster (as we discussed earlier, usually after 24 hours of meds, you’re no longer spreading germs). It’s crucial to take the full course of antibiotics – finish all the pills even if you feel better in two days. Stopping early can lead to a resurgence of the bacteria or contribute to antibiotic resistance.
In addition to antibiotics, treating strep throat includes supportive care: rest, fluids, and maybe over-the-counter pain relievers (acetaminophen or ibuprofen) for the fever and throat pain. Many of the comfort measures for viral tonsillitis (see below) also apply to strep.
- Treatment for Viral Tonsillitis: If your tonsillitis is caused by a virus, antibiotics won’t help at all. They do nothing against viruses. So treatment is all about relieving symptoms and helping your body fight it off. This includes:
- Rest: Your body needs energy to battle the virus, so take it easy.
- Hydration: Drink plenty of fluids. If it’s hard to swallow, try warm soothing liquids (herbal tea with honey, warm broth) or very cold ones (ice water, popsicles) – whatever feels better on your throat.
- Pain and fever relief: Over-the-counter meds like ibuprofen or acetaminophen can reduce throat pain and control fever. (Avoid aspirin in kids, as it’s not recommended due to risk of Reye’s syndrome).
- Saltwater gargles: Gargling warm salt water (1/2 teaspoon of salt in a cup of water) a few times a day can help reduce throat swelling and pain.
- Throat lozenges or sprays: These can soothe the throat (just avoid giving lozenges to very young children as they can be a choking hazard).
- Humidifier: Keeping the air moist with a cool-mist humidifier can prevent your throat from drying out and might ease discomfort, especially at night.
Viral tonsillitis usually gets better on its own in about a few days to a week. The above measures just make that week a bit more bearable. If symptoms are particularly severe or last longer than expected, a doctor might re-evaluate to ensure something wasn’t missed.
- What if it’s unclear? Sometimes a doctor might say, “It could be strep, could be viral; we’ll treat you with antibiotics just in case while waiting on a culture.” This is not uncommon if, for example, rapid strep is negative but suspicion remains. They may start antibiotics and later call you to stop them if the culture shows no strep. It’s always fair to ask your provider if you’re not sure why they’re giving or not giving antibiotics.
Another scenario: recurrent tonsillitis. If someone keeps getting tonsillitis (whether strep or viral) multiple times a year, doctors might discuss a tonsillectomy (surgical removal of the tonsils). This is generally considered if tonsillitis happens beyond a certain frequency (for example, seven times in one year, or five times a year for two years in a row). Removing the tonsils can dramatically cut down these infections, though it’s usually a last resort after frequent illness. This applies to both recurrent strep infections and generally recurrent tonsillitis of any cause.
Which One Is More Contagious?
Patients often ask if strep throat is more contagious than viral tonsillitis or vice versa. The answer: both can spread to others pretty easily through close contact. Regardless of cause, if someone has a throat infection, you should assume their saliva and droplets are infectious. Strep throat, being a specific bacteria, has well-known guidelines – you’re not contagious after 24 hours on antibiotics. Viral tonsillitis can vary depending on the virus, but generally you’re contagious until your symptoms improve. In practical terms, if you have a bad sore throat and fever (either cause), stay home and away from close contact with others until you’re on treatment or getting better. Use the preventive steps we described in earlier sections (handwashing, not sharing cups, etc.). Kids with strep shouldn’t go to school or daycare until the fever is gone and they’ve been 24 hours on antibiotics, and kids with viral tonsillitis should stay home until fever is gone and they’re feeling more like themselves.
One could argue strep is more contagious in group settings because it tends to cause noticeable illness and can lead to mini-outbreaks (like a classroom where several kids pass it around). But viruses like the Epstein-Barr virus (mono) are also quite contagious in their own way. So it’s best not to underestimate either. Bottom line: treat both scenarios as contagious and be careful about spreading germs.
Putting It All Together
Let’s summarize in a patient-friendly way: Tonsillitis is a broad term for inflamed tonsils, and strep throat is one specific (bacterial) cause of it. If you have a sore throat with cold symptoms, it’s likely viral tonsillitis. If you have a very severe sore throat with fever and no cough, it could be strep throat. The only sure way to know is a strep test at the doctor’s office. Strep throat needs antibiotics; viral tonsillitis needs rest and TLC. Both will usually get better, but strep treatment will speed up recovery and prevent rare complications. And importantly, both can spread to others, so taking precautions (and isolating for a bit if you’re
ill) is the kind thing to do.
In either case, if you’re ever unsure or your symptoms are very intense (like difficulty breathing or swallowing, or illness lasting too long), seek medical attention. The good news is that with proper care, most people recover from tonsillitis or strep throat within a week or so and get back to their regular life. Now you can be confident in knowing the difference between these terms and what to do about each one.
References:
- First Response Healthcare. Strep Throat vs. Tonsillitis: Key Differences and Symptoms (2024) – Explains that tonsillitis is inflammation of the tonsils from various causes, while strep throat is specifically caused by Streptococcus pyogenes. Notes that Group A strep accounts for about 30% of tonsil infections.
- American Family Care (AFC Urgent Care). Strep Throat vs. Tonsillitis: How to Tell the Difference & How to Treat It – Describes symptom overlap and differences, noting that tonsillitis (especially viral) often includes cough, runny nose, and postnasal drip, whereas strep throat typically does not and instead may present with more severe throat symptoms and rash. Also discusses that both are treated similarly in terms of symptom relief, but strep requires antibiotics.
- How do you know if tonsillitis is viral or bacterial? – Outlines distinguishing symptoms: viral tonsillitis often has cough, hoarseness, and runny nose, improving in about 4-10 days, whereas bacterial (usually strep) has severe sore throat, fever >101°F, swollen lymph nodes, and white pus on tonsils, and will persist or worsen without treatment.
- Verywell Health. Is Tonsillitis Contagious? – Clarifies that a bacterial infection causes about 15-30% of tonsillitis cases (essentially strep throat), and the rest are viral. Emphasizes the need for a rapid strep test to confirm the cause, as symptoms alone can be similar.
- Tonsillitis in Adults: What to Expect – Highlights general treatment approaches, stating that viral tonsillitis is managed with rest, fluids, and over-the-counter remedies, while recurrent or severe cases (often bacterial) might necessitate medical interventions or tonsillectomy.
- Cleveland Clinic. Tonsillitis: Symptoms, Causes & Treatment – Notes that most viral tonsillitis cases resolve in a few days with conservative care, and antibiotics typically eliminate bacterial tonsillitis (strep) in about 10 days. It reinforces that proper diagnosis is key to determine if antibiotics are needed.
- Centers for Disease Control and Prevention (CDC) – Group A Strep Guidance – Recommends testing for strep throat in patients with sudden-onset sore throat and certain clinical signs, and treating confirmed strep w
ith atibiotics to prevent complications. Advises that individuals with strep can return to school or work after 24 hours of antibiotics and no fever, to avoid spreading the bacteria.