During which phase, gram positive bacteria is most susceptible to penicillin?
Bacterial growth refers to the increase in number of bacterial cells. Bacteria divide exponentially into the environment. Bacteria growth is represented in the form of generation time. Generation time is the time in which the bacterial cell divides into two.
Bacterial division:
Bacteria divide through the process of:
- Binary fission: Binary fission is the most common method in the division of bacteria. Bacteria replicate its genetic material into the cell. The chromosomes duplicate and cell membrane start pinching inward the membrane. This invagination results in the formation of a new daughter cell. Peptidoglycan starts to accumulate in the membrane and form the cell wall. The cell wall formation forms the new independent cell.
- Fragmentation: Fragmentation refers to the formation of a new cell from the fragment of the filamentous bacteria. The filamentous bacteria cut into fragments. The new fragment starts growing into the new bacterial cell. This process is common in filamentous bacteria.
- Budding: Budding is the process in which the bud grows into a new bacterial cell. The bud may either remain attached or de-attach from the parent cell. This bud grows into a new offspring.
Bacterial growth phases:
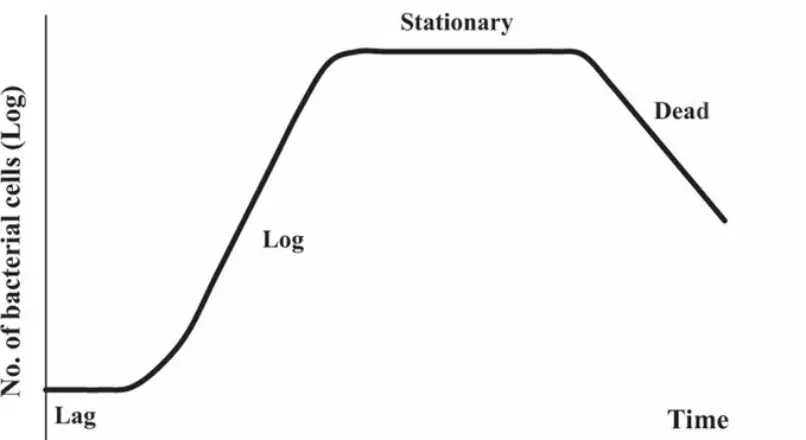
The logarithm analysis is done by growing the bacteria into the broth culture. That analysis showed that bacterial growth occurs in four phases.
- Lag phase
- Log phase
- Stationary phase
- Decline phase

Lag phase:
It is the growth phase in which the bacteria prepare itself for growth. During this phase, bacteria
- Grow in size
- Don’t undergo binary fission
- Prepare its cells for enzymes
- Prepare ribosomes and cellular component for the cell division.
- Growth is restricted.
Log phase:
It is the growth phase in which the bacteria starts growing exponentially. During this phase, bacteria
- Increase its cell number
- Undergo binary fission
- Utilize all the enzymes for the division that are synthesized in lag phase
- Prepare the proteins for cell
- Growth is not restricted
- Cell size is small and uniform
- represent as generation time of bacteria
Stationary phase:
It is the phase in which the bacteria death also occur. During this phase,
- No net increase or decrease in cell number
- The number of division is equal to the number of cell death
- Available of limited nutrient
- Lack of space in the culture
- Preparation of secondary metabolites
- Due to the storage of granules, variable staining is done.
Death phase:
It is the phase in which the bacteria death occur. During this phase,
- Increase in the number of bacterial death
- Unavailability of nutrients for growth
- Increase in secondary metabolites
Penicillin:
Penicillin is the beta-lactam antibiotic that is used for gram-positive bacteria. It inhibits the cell wall synthesis and directly targets the cell wall of bacteria. It is a narrow spectrum antibiotic that is used for the gram-positive bacteria. It contains a beta-lactam ring that is responsible for its activity. Penicillin is the first antibiotic that was discovered by Alexander Fleming. Penicillin is naturally synthesized by a fungus, Penicllium chrysogenum. He observed that there is a clear zone of inhibition of bacteria where the fungus growth. He isolated the fungus metabolite that kills the bacteria and named as penicillin. Penicillin has the bactericidal effect that kills the bacteria.
Mode of action:
Penicillin is a cell wall inhibitor. The cell wall is composed of peptidoglycan subunits. This peptidoglycan is the polymers of sugar and amino acids. The sugar N-acetylglucosamine and N- acetylmuramic acid linked with the amino acids. Three to five peptide chains linked the sugar and protein together. These polymers combine to give the structure of the bacterial cell. Peptidoglycan creates a mesh-like appearance that prevents the extracellular component to move inside the cell. Penicillin works by targeting the peptidoglycan. Penicillin attacks the peptidoglycan subunit of the cell wall. The cell wall breaks that leads to the weakening of the cell. When bacteria multiply, small holes create that are not fill by peptidoglycan. The weak cell wall can’t support bacterial growth. Bacteria live in a watery environment and water moves inside the cell. When water enters, bacterial cell burst and die.
Types of penicillin:
There are five types of penicillin that are used nowadays for the prevention of disease.
- Natural penicillin
- Carboxy-penicillin
- Amino-penicillin
- Urido-penicillin
- Beta-lactamase resistant penicillin
When bacteria uptake the antibiotics?
Bacterial growth occurs in 4 phases as described above. But, gram-positive bacteria are susceptible during the log phase of the bacterial growth. During log phase, bacteria are sensitive because
- Bacteria grow exponentially and increase their cell mass.
- The cell is small in size.
- The cell produces its proteins, amino acids and other precursor units.
- The cell membrane is less permeable at that time because the cell needs nutrient from the environment.
- When nutrients are taken up by the cell, antibiotics also move inside the cell.
- Penicillin when enter, it degrades its cell wall subunit.
- Bacterial cell become weak and die
- This phase is medically important as in this phase, bacteria are sensitive to drugs.
Resistance:
But nowadays, many bacteria are resistant to antibiotics. Mostly gram-negative bacteria are resistant to penicillin and penicillin don’t act on them. There are two types of resistance in bacteria.
- Natural resistance is the type in which the bacteria are naturally resistant to the antibiotics. It is non-transferable to the other bacteria. For example; gram-negative bacteria have small peptidoglycan content, so penicillin doesn’t work on them.
- Acquired resistance is the type in which bacteria acquired or adapted resistant from the environment. When antibiotics are used for the long term, the bacteria become resistant to them. This resistant is transferable to other bacteria and most of the bacteria acquired resistant from the misuse of antibiotics.
Resistance mechanism:
There are three commonly resistant mechanisms that are adapted by gram-positive bacteria for survival.
- Penicillinase enzyme: Bacteria synthesize the Penicillinase enzymes that degrade the penicillin ring. Penicillin antibiotic activity depends on the beta-lactam ring. When the ring is broken by enzymes, its activity stop and bacteria survive in the environment.
- Modification of target site: Antibiotics always work by binding to its target site. Bacteria change its target site for the antibiotics. When the target sites are changed, antibiotics are unable to bind with them. The unbinding of antibiotic with the target site destroys the effect of the antibiotic.
- Efflux pumping: Bacteria have some modified proteins that pump the penicillin out from the cell. When penicillin moves out, bacteria survive and able to grow.
Leave a reply